What To Do If You Get Hypothermia
As the winter season blankets the landscape with snow and chills the air, it brings with it the serene beauty of frost-covered landscapes and the promise of outdoor adventures. However, amidst the picturesque scenes and exhilarating activities, it's crucial to remain mindful of the potential dangers posed by the cold. In these frigid temperatures, the risk of cold-related injuries such as hypothermia becomes all too real.
To ensure a safe and enjoyable winter experience, it's essential to understand the knowledge and strategies needed to combat hypothermia. From signs and symptoms to the importance of proper layering and moisture management, we'll cover a range of topics to help you navigate this medical emergency. Whether you're planning a backcountry skiing excursion, a winter camping trip, or simply braving the elements on your daily commute, our guide provides valuable insights to help you mitigate the risks associated with hypothermia.
What is hypothermia?
Picture this: You're out on a winter hike, surrounded by the serene beauty of snow-covered trees and crisp, chilly air. As you venture deeper into the wilderness, your body is working hard to keep you warm, generating heat to combat the cold temperatures. But what if the cold wins? That's where hypothermia comes into play. It occurs when your body loses heat faster than it can produce it, causing your core temperature to plummet below its normal level. It's like a battle between your body's ability to generate warmth and the relentless chill of the environment. This imbalance typically happens during prolonged exposure to cold conditions, gradually depleting your body's energy reserves as it struggles to maintain its internal heat.
Think of hypothermia as a warning sign from your body, signaling that it's overwhelmed by the cold and needs immediate attention. Ignoring it can have serious consequences, which is why understanding the mechanisms behind hypothermia is crucial, especially for outdoor enthusiasts like hikers, campers, and skiers.
But here's the kicker: Hypothermia isn't just a concern in freezing temperatures. Even in cooler temperatures above 40 degrees Fahrenheit, factors like rain, sweat, or being submerged in cold water can rapidly sap your body's warmth, putting you at risk. So, whether you're enjoying a winter hike or hitting the slopes, being aware of hypothermia and taking preventive measures can make all the difference in keeping your outdoor adventures safe and enjoyable.
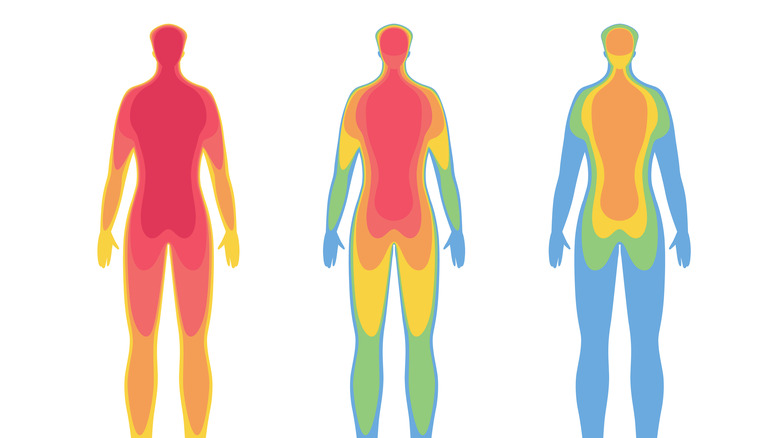
Recognizing the signs
In the early stages of hypothermia, the signs may be subtle and easy to miss. According to the Better Health Channel, at this stage, skin may appear pale and feel cool to the touch. Numbness in the extremities, such as fingers and toes, can accompany this stage, alongside sluggish responses, drowsiness, or a general sense of lethargy. Shivering is common as the body attempts to generate heat, and there may be an increase in heart rate and breathing as the body works harder to regulate temperature.
As hypothermia progresses into the moderate stage, the signs become more pronounced, reflecting the body's increasing struggle to maintain its core temperature. Shivering ceases as the body's ability to produce heat diminishes, and there is a notable slowing of heart rate and breathing rate. Individuals may experience a decrease in consciousness too.
In the most severe stage of hypothermia, the signs and symptoms paint a dire picture of the body's critical state. Individuals may lose consciousness entirely, becoming unresponsive to external stimuli. The heart beats more slowly and may even become irregular, signaling imminent danger of cardiac arrest if the body continues to cool. No response to light in the pupil of the eye, along with rigid muscles resembling rigor mortis, further underscore the severity of the situation. Although pulses and respiratory effort may still be present, they can be difficult to detect, indicating a need for immediate medical attention to reverse the potentially fatal consequences of severe hypothermia.
Find or create shelter
Ensuring adequate shelter, whether it's finding natural protection or creating makeshift cover, is paramount in the fight against hypothermia, especially in outdoor settings where exposure to cold weather is a risk. Shelter serves as a crucial barrier against the elements, helping to retain body heat and prevent further cooling. In fact, a study in the International Journal of Environmental Research and Public Health found that people without homes are disproportionately affected by hypothermia, underscoring the importance of shelter in preventing this condition.
Natural shelters such as caves, rock overhangs, or dense vegetation provide immediate refuge from wind and precipitation, significantly reducing heat loss from the body. In emergency situations, the ability to quickly locate and utilize these natural features can be lifesaving. In instances where natural shelter is unavailable, it's imperative to create temporary refuge. Building a shelter using available materials such as branches, foliage, and even snow can provide life-saving protection from the elements. Simple structures like lean-tos, debris shelters, or snow caves offer effective insulation and can help retain body heat, mitigating the risk of hypothermia.
Moreover, shelter not only provides physical protection but also offers psychological comfort and stability. In stressful situations, having a safe haven to retreat to can alleviate anxiety and promote a sense of security, which is crucial for maintaining mental resilience in challenging conditions.
Remove wet clothing
Wet garments exacerbate heat loss, which is why removing wet clothing is a critical step in overcoming hypothermia. When clothing becomes wet, whether due to precipitation, immersion in water, or sweat, it compromises the insulating properties of the fabric. Moisture trapped against the skin creates a chilling effect, causing the body to lose heat rapidly. This process, known as conduction, can lead to a dangerous drop in core body temperature, especially in cold or windy conditions. Moreover, wet clothing can impede the body's ability to regulate temperature effectively. As moisture evaporates from the fabric, it draws heat away from the skin. This further contributes to cooling and can exacerbate the risk of hypothermia, particularly when coupled with other factors such as wind or low ambient temperatures.
By replacing damp garments with dry layers, you can reduce heat loss and restore thermal balance. In fact, a study published in Wilderness & Environmental Medicine found that wet clothing removal is associated with an accelerated rate of skin rewarming in comparison to merely adding more layers. In situations where dry clothing is unavailable, efforts should be made to dry wet garments using available resources such as body heat, sunlight, or fire. Wringing out excess moisture and allowing clothing to air dry can also help restore insulation and reduce heat loss.
Use body heat to re-warm up
Using body heat to apply warmth to someone's core when they are experiencing hypothermia is a common practice in emergency situations where conventional heating methods may not be readily available. This technique involves direct contact between an individual with a normal body temperature (the donor) and the hypothermic person (the recipient) to transfer heat and aid in rewarming, with a particular focus on the core, where the majority of our vital organs rest. The concept behind body-to-body rewarming is to utilize the natural heat generated by an individual to raise the core temperature of the hypothermic person. This process typically occurs within an insulated environment, such as a sleeping bag or emergency blanket, to minimize heat loss to the surroundings.
While body-to-body rewarming can be effective in certain situations, its efficacy may vary depending on factors such as the severity of hypothermia, the duration of exposure to cold, and the ambient conditions, as found by a study in the Journal of Applied Physiology. Despite its potential drawbacks, body-to-body rewarming remains a valuable tool in the arsenal of hypothermia treatment, especially in remote or resource-limited settings where alternative heating options are limited. When implemented properly and in conjunction with other medical interventions, such as passive rewarming and gradual rehabilitation, body heat transfer can play a crucial role in stabilizing hypothermic individuals and improving their chances of recovery.
Drink warm liquids
When facing the chilling threat of hypothermia, sometimes the most effective solutions come in the simplest forms. Among these is the often underestimated power of warm liquids. While it may seem like a small comfort in the face of such a serious condition, drinking warm liquids can play a significant role in aiding the body's fight against hypothermia.
First and foremost, warm liquids provide an immediate source of heat to the body from within. By ingesting warm fluids such as hot tea, cocoa, or broth, you can quickly raise their internal temperature, helping to counteract the effects of hypothermia. This internal heat generation can be particularly beneficial in situations where external heating methods are limited or unavailable.
Moreover, warm liquids serve to hydrate the body, which is essential for maintaining proper physiological function, especially in cold environments. Dehydration can exacerbate the symptoms of hypothermia and hinder the body's ability to regulate temperature effectively, which is why alcohol is not recommended for a hypothermic person. By ensuring adequate fluid intake, you can support their body's natural processes and improve their overall resilience against the cold.
Monitor vital signs
Monitoring vital signs during hypothermia requires special attention and care due to the body's altered physiological state. First, measuring core body temperature is crucial in assessing the severity of hypothermia and guiding treatment. The most accurate method of measurement is a thermometer. Otherwise, skin-to-skin contact can help determine a person's temperature. The skin also provides insights into circulation. Pale, cold, or clammy skin may indicate poor circulation and reduced blood flow to the extremities.
If on hand, a heart rate monitor can provide real-time data on pulse rate, while a blood pressure cuff can be used to measure blood pressure periodically. Alternatively, counting beats per minute while feeling someone's wrist or neck pulse is a viable option (per Johns Hopkins Medicine, 60 to 100 beats is a normal pulse for a healthy adult). The same can be done to check respiratory rate (an adult at rest will make around 12 to 16 breaths per minute). Changes in heart rate, breathing rate, and blood pressure may indicate worsening hypothermia or other complications.
Lastly, assessing pupil size and reactivity to light can provide information about neurological function and potential brain injury. Pupils that are dilated, sluggish, or non-reactive may indicate neurological impairment and the need for further evaluation. The same may be true if a hypothermic person exhibits changes in consciousness or confusion.
Do not massage limbs
While it may seem intuitive to massage the limbs of someone experiencing hypothermia to increase circulation and warmth, this approach can actually do more harm than good. In hypothermic individuals, the tissues are already at risk of damage due to reduced blood flow and oxygen delivery. Friction from massage can damage delicate blood vessels and exacerbate tissue damage.
We know well by now that hypothermia slows down metabolic processes and impairs cardiac function. Vigorous massage of cold limbs can stimulate, causing an influx of blood away from the core. This can trigger a potentially dangerous drop in core body temperature, leading to arrhythmias or even cardiac arrest. Thus, rather than promoting effective rewarming, massaging cold limbs can delay the process by disrupting the body's natural mechanisms for heat retention and distribution.
In addition, hypothermic individuals may already be experiencing pain and discomfort due to cold exposure and tissue damage. Massaging cold limbs can exacerbate this pain and cause further distress. Instead of providing relief, vigorous massage may intensify sensations of numbness, tingling, or burning, making the individual's experience even more uncomfortable.
Perform gentle, active movements in mild cases only
In cases of mild hypothermia, where the individual is conscious and able to move without difficulty, gentle movement can help stimulate blood flow and promote heat generation. Gentle exercises, such as slow, controlled stretches, can help increase circulation and generate heat. This can aid in the rewarming process and prevent further cooling. Or if rewarming has begun and the individual's core temperature starts to rise, gentle movement can aid in recovery and rehabilitation. Notably, easy movements can help restore muscle function, improve circulation, and prevent stiffness or joint pain associated with prolonged immobility during hypothermia.
In cases of moderate and severe hypothermia where the individual's vital signs are weak or they are so cold that they are unable to even shiver, movement should be gentle and only when necessary. The same is true if they come in and out of unconscious or experience altered mental status. Even secondary movement, wherein a person moves the hypothermic person's muscles for them, can increase the risk of complications, such as cardiac arrest or exacerbation of cold-related injuries.
Evacuate if necessary
Evacuation becomes imperative in certain hypothermia scenarios. Of course, severely hypothermic individuals should be evacuated immediately. For mild cases, if on-site interventions — such as rewarming techniques or supportive measures — fail to improve the individual's condition or if their symptoms worsen despite treatment, evacuation should be considered. Timely evacuation ensures access to advanced medical care and facilities that can better manage severe cases of hypothermia. However, it is important to note that in remote or wilderness settings where access to medical resources or proper shelter is limited, evacuation may be necessary even at the onset of mild cases of hypothermia. Sometimes, these cases can worsen without access to medical aid.
Before evacuation, ensure the individual is adequately stabilized to withstand transportation. This may involve continuing rewarming efforts, providing insulation with blankets or sleeping bags, and protecting them from further exposure to cold or adverse weather conditions. Evacuate the individual using the safest and most appropriate means of transportation available. Depending on the location and terrain, this could involve carrying the individual on a stretcher, using a vehicle, or utilizing specialized rescue equipment, such as helicopters or snowmobiles. Throughout the evacuation process, vigilantly monitor the individual's vital signs and overall condition. Provide reassurance and support to alleviate anxiety and discomfort, and be prepared to intervene promptly if their condition deteriorates during transport.
Seek medical attention
Seeking medical attention is crucial after experiencing hypothermia, even if you start to feel better and is able to continue and finish their excursion. Hypothermia can have serious implications for health, and a thorough medical evaluation is essential to ensure that no underlying complications exist and to prevent future occurrences.
In milder cases, while the immediate symptoms of hypothermia may improve with rewarming and rest, there could be underlying complications that require medical attention. These complications include frostbite, respiratory issues, cardiac abnormalities, or neurological impairments that may display themselves later on. A healthcare professional can conduct a comprehensive assessment to identify any potential complications and provide appropriate treatment.
Another consideration you need to consider after experiencing hypothermia is afterdrop. Afterdrop refers to a drop in core body temperature that can occur during the rewarming process or after you have been rewarmed. This phenomenon can lead to a delayed onset of hypothermia-related symptoms or exacerbate existing symptoms. Medical supervision is crucial to monitor for signs of afterdrop and ensure that your core temperature remains stable.
Tips for prevention
Dressing appropriately is crucial for staying warm and preventing hypothermia. It's recommended to wear multiple layers of clothing, starting with a moisture-wicking base layer to draw sweat away from the skin. Over this, add insulating mid-layers to trap heat close to the body, and finally, a waterproof and windproof outer layer to protect against the elements. Choosing clothing made from materials such as wool or synthetic fibers is ideal, as they retain heat even when wet. Additionally, don't forget to cover your extremities with gloves, hats, and warm socks to prevent heat loss from these areas.
Staying hydrated and well-nourished is important for fueling your body's heat production. Dehydration and hunger can impair your body's ability to regulate temperature, so it's essential to stay hydrated and well-fed, especially in cold weather conditions. Drink plenty of fluids, such as water or warm beverages, and eat high-energy foods to keep your body fueled and warm. The Red Cross recommends avoiding alcohol and caffeine since they can impair your body's ability to regulate temperature.
Take regular breaks during outdoor activities in cold weather to allow your body to rest and recover, reducing the risk of hypothermia. Seek shelter indoors or in a warm, sheltered area to warm up periodically. This gives your body a chance to re-energize and maintain its core temperature, preventing excessive heat loss and reducing the risk of hypothermia.